Respiratory sounds
This article needs additional citations for verification. (May 2015) |
| Respiratory sounds | |
|---|---|
| Other names | Breath sounds, lung sounds |
 | |
| Specialty | Respirology |
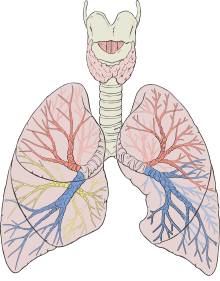
Respiratory sounds, also known as lung sounds or breath sounds, are the specific sounds generated by the movement of air through the respiratory system.[1] These may be easily audible or identified through auscultation of the respiratory system through the lung fields with a stethoscope as well as from the spectral characteristics of lung sounds.[2] These include normal breath sounds and added sounds such as crackles, wheezes, pleural friction rubs, stertor, and stridor.
Description and classification of the sounds usually involve auscultation of the inspiratory and expiratory phases of the breath cycle, noting both the pitch (typically described as low (≤200 Hz), medium or high (≥400 Hz)) and intensity (soft, medium, loud or very loud) of the sounds heard.[3]
Normal breath sounds
[edit]Normal breath sounds are classified as vesicular, bronchovesicular, bronchial or tracheal based on the anatomical location of auscultation.[4][3] Normal breath sounds can also be identified by patterns of sound duration and the quality of the sound as described in the table below:[4]
| Name | Location where heard normally | Quality of sound | Sound duration | Example |
|---|---|---|---|---|
| tracheal | over the trachea | very loud | expiratory sound duration is equivalent to inspiratory sound | |
| bronchial | over the manubrium | loud, high pitched | expiratory sound duration is longer than inspiratory sound | |
| bronchovesicular | anteriorly between the 1st and 2nd intercostal space;
posteriorly in-between the scapulae |
intermediate | expiratory sound duration is about equivalent to inspiratory sound | |
| vesicular | over most of both lungs | soft, low pitched | expiratory sound duration is shorter than inspiratory sound |
Abnormal breath sounds
[edit]Common types of abnormal breath sounds include the following:[5]
| Name | Continuous/discontinuous | Frequency/pitch | Inspiratory/expiratory | Quality | Common Causes | Example |
|---|---|---|---|---|---|---|
| Wheeze or rhonchi | continuous | high (wheeze) or lower (rhonchi) | expiratory or inspiratory | whistling/sibilant | Caused by narrowing of airways, such as in asthma, chronic obstructive pulmonary disease, foreign body. | |
| Stridor | continuous | high | inspiratory, expiratory, or both[6] | whistling/sibilant | epiglottitis, foreign body, laryngeal edema, croup | |
| Inspiratory gasp | continuous | high | inspiratory | whoop | pertussis (whooping cough) | see New England Journal of Medicine, Classic Whooping Cough sound file, Supplement to the N Engl J Med 2004; 350:2023-2026 |
| Crackles (rales) | continuous | high (fine) or low (coarse) | inspiratory | cracking/clicking/rattling[7] | pneumonia, pulmonary edema, tuberculosis, bronchitis, heart failure | |
| Pleural friction rub | discontinuous | low | inspiratory and expiratory | many repeated rhythmic sounds | inflammation of lung linings, lung tumors | not available |
| Hamman's sign (or Mediastinal crunch) | discontinuous | neither (heartbeat) | crunching, rasping | pneumomediastinum, pneumopericardium | not available | |
| Grunting | Continuous | low | expiratory | snoring | surfactant deficiency, pneumonia, cardiac abnormalities[8] |
Continued
[edit]- Rales: Small clicking, bubbling, or rattling sounds in the lungs. They are heard when a person inhales. They are believed to occur when air opens alveoli. Rales can also be described as moist, dry, fine, and coarse.[9]
- Rhonchi are coarse rattling respiratory sounds, usually caused by secretions in bronchial airways. The sounds resemble snoring. "Rhonchi" is the plural form of the singular word "rhonchus".[8]
- Stridor: Wheeze-like sound heard when a person breathes. Usually it is due to a blockage of airflow in the windpipe (trachea) or in the back of the throat.[10]
- Wheezing: High-pitched sounds produced by narrowed airways. They are most often heard when a person breathes out (exhales). Wheezing and other abnormal sounds can sometimes be heard without a stethoscope.[11]
Other tests of auscultation
[edit]
Pectoriloquy, egophony and bronchophony are tests of auscultation that utilize the phenomenon of vocal resonance.[3] Clinicians can utilize these tests during a physical exam to screen for pathological lung disease. For example, in whispered pectoriloquy, the person being examined whispers a two syllable number as the clinician listens over the lung fields. The whisper is not normally heard over the lungs, but if heard may be indicative of pulmonary consolidation in that area. This is because sound travels differently through denser (fluid or solid) media than the air that should normally be predominant in lung tissue. In egophony, the person being examined continually speaks the English long-sound "E" (/i/). The lungs are usually air filled, but if there is an abnormal solid component due to infection, fluid, or tumor, the higher frequencies of the "E" sound will be diminished. This changes the sound produced, from a long "E" sound to a long "A" sound (/eɪ/).
History
[edit]In 1957, Robertson and Coope proposed the two main categories of adventitious (added) lung sounds. Those categories were "Continuous" and "Interrupted" (or non-continuous).[12] In 1976, the International Lung Sound Association simplified the sub-categories as follows:
Several sources will also refer to "medium" crackles, as a crackling sound that seems to fall between the coarse and fine crackles. Crackles are defined as discrete sounds that last less than 250 ms, while the continuous sounds (rhonchi and wheezes) last approximately 250 ms. Rhonchi are usually caused by a stricture or blockage in the upper airway. These are different from stridor.
See also
[edit]References
[edit]- ^ "Breath sounds: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2021-11-11.
- ^ Sengupta, Nandini; Sahidullah, Md; Saha, Goutam (August 2016). "Lung sound classification using cepstral-based statistical features". Computers in Biology and Medicine. 75 (1): 118–129. doi:10.1016/j.compbiomed.2016.05.013. PMID 27286184.
- ^ a b c Zimmerman, Barret; Williams, Donna (2021), "Lung Sounds", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30725938, retrieved 2021-11-11
- ^ a b Bickley, Lynn S (2013). Bates' Guide to Physical Examination and History-Taking. Wolters Kluwer Health/Lippincott Williams & Wilkins. pp. 311–312. ISBN 978-1609137625.
- ^ Bohadana, Abraham (February 20, 2014). "Fundamentals of Lung Auscultation". New England Journal of Medicine. 370 (8): 744–751. doi:10.1056/NEJMra1302901. PMID 24552321. S2CID 17871815.
- ^ Leung, Alexander K. C.; Cho, Helen (1999-11-15). "Diagnosis of Stridor in Children". American Family Physician. 60 (8): 2289–2296. ISSN 0002-838X. PMID 10593320.
- ^ "Breath sounds: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2022-05-06.
- ^ a b McGann, Kathleen A.; Long, Sarah S. (2018-01-01), Long, Sarah S.; Prober, Charles G.; Fischer, Marc (eds.), "21 - Respiratory Tract Symptom Complexes", Principles and Practice of Pediatric Infectious Diseases (Fifth Edition), Elsevier, pp. 164–172.e2, ISBN 978-0-323-40181-4, retrieved 2022-05-06
- ^ "Breath sounds: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2022-05-30.
- ^ "Stridor: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2022-05-30.
- ^ "Breath sounds: Medline Plus". NIH. Retrieved 5 May 2015.
- ^ Robertson, A (1957). "Rales, rhonchi, and Laennec". Lancet. 2 (6992): 417–23. doi:10.1016/S0140-6736(57)92359-0. PMID 13464086.
- ^ American Thoracic Society Ad Hoc Committee on Pulmonary Nomenclature (1977). "Updated nomenclature for membership reaction". ATS News (3): 5–6.
- ^ Loudon, R; Murphy, R (1984). "Lung Sounds". Am Rev Respir Dis. 130 (4): 663–73. doi:10.1164/arrd.1984.130.4.663 (inactive 2024-09-12). PMID 6385790.
{{cite journal}}: CS1 maint: DOI inactive as of September 2024 (link)
Mansy, H. A.; Royston, T. J.; Balk, R. A.; Sandler, R. H. (2002). "Pneumothorax detection using computerised analysis of breath sounds". Medical & Biological Engineering & Computing. 40 (5): 526–532. doi:10.1007/BF02345450. PMID 12452412. S2CID 7413897.
External links
[edit]- Audio Breath Sounds Archived 2020-12-15 at the Wayback Machine - Multiple case studies with audio files of lung sounds.
- R.A.L.E. Repository - sound files of breath sounds
- MEDiscuss - Respiratory auscultation with audio examples
- Wilkins R, Dexter J, Smith J (1984). "Survey of adventitious lung sound terminology in case reports". Chest. 85 (4): 523–5. doi:10.1378/chest.85.4.523. PMID 6705583.
- Lehrer, Steven. Understanding Lung Sounds. Elsevier 2002.
- Lung Sounds - 20 recordings and waveforms

